Critical Care team honoured with double award win
A team at Blackpool Victoria Hospital have been talking of their delight in winning two internal awards.
The Critical Care team, clinched the Clinical Team of the Year and Chairman’s Award in the Blackpool Teaching Hospitals NHS Foundation Trust Celebrating Success Awards held virtually, earlier this month.
Their success was as a result of a heart-warming nomination describing the incredible level of care within the Intensive Care and High Dependency Units, collectively known as Critical Care, during the COVID pandemic.
Sister Rosie Spencer, who has worked in the department for eight years, said: “So many people did so much and are still doing so much during the COVID pandemic.
“As we were watching the awards ceremony live. We started to think we may win. When Medical Director, Dr Jim Gardner described the team before announcing the winner, we started to feel emotional. We are all very proud to have this recognition. COVID has brought the team even closer together as we have shouldered the hard times together.”
When the COVID hit in 2020 it was only a matter of days before the unit was full. At the time, nobody really knew what to expect. Nobody had dealt with a pandemic of this scale before.
Clinical Matron for Critical Care, Karen Smith, said: “Once visiting was suspended to try and ease the spread of the virus, relationships with patients and families grew closer and virtual visiting was introduced.
“Despite working under immense pressure, the team surpassed all expectations by buying newspapers, toiletries, baking cakes for special birthdays so the patients felt special especially as they were not allowed visitors.”
As days turned into weeks and months, some patients did not recover. Soon the team had to approach difficult conversations about end of life.
Karen added: “Despite the emotional toll, the team’s compassion shone out, holding patients’ hands in theirs whilst virtually comforting relatives. Suffering the torment of hearing a family saying their last goodbyes, feeling like an intruder but promising families their loved one would not die alone.”
The team also ensured that touching mementoes such as locks of hair, handprints and photographs were sent back to families to help them grieve.
Ward Manager for HDU and ITU, Amy Cartmell, said: “Working within this unit for the last 12 years, I have always been immensely proud to be part of the Critical Care family, but the last two years has been another level.
“The strength and commitment shown from every single member of the team has blown me away. This has been the hardest time we have ever faced, and it has made us even stronger than before.
“These memories and emotions will stay with us forever, and the bond within the team will only get stronger. For us to receive these awards, it feels like recognition of hard work and struggle that has been faced behind closed doors.”
You can watch The Critical Care team winning their award and the whole Celebrating Success Awards 2022 ceremony here: https://youtu.be/pciYAZnj9JY
“Each time I finish my shift, I go home knowing that we have done everything we can.”
Victor and PasqualeThanks to funding by Health Education England, the Critical Care Department has been able to put some of their staff on a Master’s degree apprenticeship course, enabling nurses to become Advanced Critical Care Practitioners (ACCP). Let’s meet two of them…
Pasquale Sarno from Naples, joined the Blackpool Victoria team in 2014 in the gastroenterology department before transferring to Critical Care as a staff nurse in 2016. Pasquale was a Critical Care nurse in his native Italy before learning English and working for the NHS.
Victor Quiatchon joined the NHS in 2010 after nursing in the Philippines. He joined Blackpool Victoria Hospital as a healthcare assistant and needed further study to qualify as a nurse in the NHS.
Victor worked in the respiratory ward before joining the Intensive Care Unit (ICU) in 2012 as a senior Band 5 nurse.
As trainee ACCPs, their work and studies are governed by four areas: Clinical Decision Making; Leadership; Education and Research. Their studies will run for three years and once qualified in 2021, they will provide care that is the bridge between a senior nurse and a doctor.
Victor said: “I thought I knew a lot before I started this programme, but we have started at the bottom, which was daunting at first. But we help each other and have some amazing support from senior doctors and the wider team.”
The two year course, run by the University of Salford, is not for the faint hearted. They must complete 25 hours of clinical practice, attend university for 15 hours and study for 30-40 hours per week.
Pasquale said: “The course is set up to fulfil the needs of Critical care patients. In Critical care, there is a different ratio to other wards. We have more contact with the patients and their family and get to know them very well. It can be stressful watching patients lose their battles but we look after each other. It’s like one big family.”
Victor added: “Here we cater for more complex needs and treatment is planned and given very quickly. We really have embraced a tough new challenge, but each time I finish my shift, I go home knowing that we have done everything we can.”
“Pasquale and I are currently on our second year of training, so far making good progress both academic and clinical.
“At this stage, our training role is more challenging as we are involved in invasive line insertions with supervision. As we progress we become more exposed with patients and do advance assessments in patient care together with our mentor consultants.
“Above this pressure clinically, our academic work is more intense as the level of assessments becomes rigid and we are expected to practice on top of everything. Pasquale and I have been supporting each all the way.”
Critical Care Voices: Team spirit is the key for Rosie
Sister Rosie Spencer has been caring for the critically ill since 2013.
She chose to nurse in Blackpool Victoria Hospital’s Critical Care department which consists of the Intensive Treatment Unit (ITU) and High Dependency Unit (HDU) as she finds the role fulfilling.
Rosie said: “Nursing in these departments gives you the satisfaction that you have done everything you possibly can for you patients.
“Have worked previously on other wards, I thought I would miss the level of patient interaction, but instead, we get to know the patient and their families really well because of the length of time that they are with us. They often keep in touch and tell us of their progress.”
Rosie has recently been promoted from staff nurse to sister which means her duties include taking charge of the unit to make sure the patients are cared for, managing patient flow and meeting the national care standards.
Of course the Covid-19 pandemic has brought a challenging time in the unit. Rosie continued: “As we are only a small unit, we have developed an even stronger team spirit.
“We are a friendly team and have welcomed many colleagues who have joined us through the pandemic. Our camaraderie has kept us going. We have really taken the team’s health and wellbeing seriously and there has been support for us all every step of the way. Most days I think ‘that’s a good team.’”
Critical Care Voices: Staff Nurse Hayley swaps roles in Covid fight
Staff nurse Hayley Willoughby recently swapped her role from theatres to critical care in order to help colleagues during the first wave of Covid-19 (coronavirus).
After qualifying in 2011, Hayley spent her first few years as an anaesthetic and recovery nurse. When the coronavirus outbreak hit earlier this year, Hayley volunteered to join the critical care team.
She said: “When the pandemic hit the hospital, I thought to myself that people need to help out and I volunteered straight away.
“Even though I have been nursing for many years, I have extra training each week to learn the critical care specialty, but this allows me to look at a patient holistically and have the autonomy to make a number of decisions about patient care.”
Having worked in theatres, Hayley already knew the consultants in critical care as they are also anaesthetists which helped her feel at home straight away
She said: “I work in a small team here and everyone knows everyone and everyone supports each other, especially in challenging times.
“The hardest part of my job at the moment is seeing patients losing their lives without any relatives being present. This is heart breaking, but we ensure that nobody is alone.”
Hayley is looking forward to working on the new unit. She said: “It is great to be looking forward and making positive changes in the department. I’ve joined the team at the right time as there is lots of change.
“What won’t change though is going home after each shift knowing you have made such a difference to a patient and their family. It’s a huge source of satisfaction.’’
“The care I received was absolutely brilliant – they saved my life.” Eddie’s Critical Care story
A patient who was critically ill in Blackpool Victoria Hospital has been describing his ordeal and determination to make a full recovery.
Eddie Haigh, 49, from Staining, suffered life threatening organ failure through sepsis following admission from a flu-related chest infection.
The father of three ended up being put into an induced coma in February after dialling 111 when he was concerned about breathing difficulties that ended up being pneumonia that left him weak and unable to walk.
He said: “My son and wife were already in bed with flu which I ultimately caught. As they got better, I seemed to get worse to the point where I thought ‘this is really serious’.
“The 111 service sent an ambulance and by this time I couldn’t even walk. I was seen very quickly in the Emergency Department where a Critical Care Consultant stayed with me and told me they may have to put me to sleep. I woke up two weeks later.”
When Eddie started to come around from his coma, that’s when the real trauma set in.
He said: “I became aware of the tubes and wires coming out of me and was fighting for every breath. It was the scariest thing in my entire life.
“I had hallucinations where it seemed that I was being killed and nothing made sense – it was a very frightening time. I don’t think people realise what you go through in this situation and there is nothing you can do to stop it.”
Eddie started his recovery having lost almost five stone and being so weak he was unable to do most things. But he was determined to improve.
He said: “It has taken some time to process what I have been through, but I am getting support with that. It was like being an 80 year-old – even my hair fell out at one point.
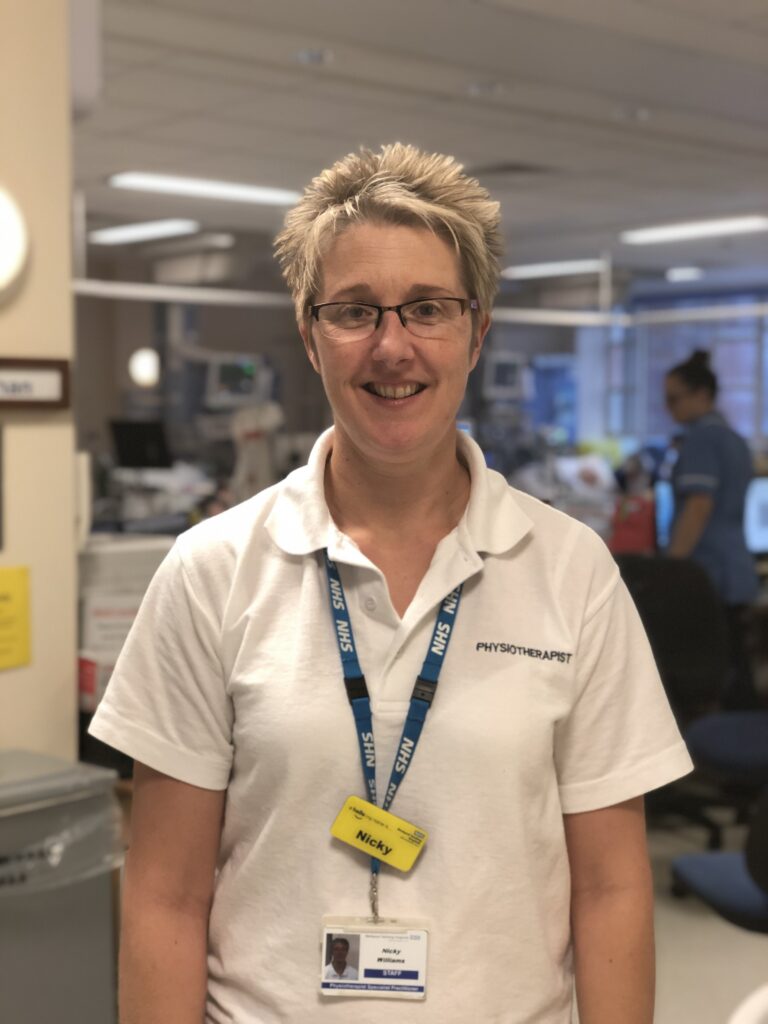
“Specialist Physiotherapist Nicky Williams has been really supportive and pushed me quite hard at times. But she has made sure that I have had the therapy I needed to be stronger and to be able to manage at home. I was so desperate to get out of hospital.”
Eddie spent a total of 52 days in hospital following a couple of setbacks in his recovery. He continued to get stronger and now follows an exercise programme that includes using weights and swimming.
Eddie said: “I have definitely built up my strength but my stamina still needs work. I still get exhausted and need a two and a half hour sleep in the daytime.
“What happened to me has definitely changed my life and priorities. I want to give back and hope to set up a blog and support group for others that have been in a similar situation.
“The care I received was absolutely brilliant – they saved my life. Staff even supported my wife Sally through my stay with hugs and kind words when they were needed.
“I was lucky. I had a lot of support from my family. I know not everyone has that and that makes me even more determined to make a difference and help others who find themselves in need of critical care.”
Eddie has just returned to his IT Consultant job on a phased and flexible return basis.
Critical Care Voices: Meet Specialist Physiotherapy Practitioner, Nicky
Over the coming weeks, we will be highlighting the roles of the people who work within the Emergency Department and Critical Care as part our Emergency Village and Critical Care Development campaign. Here we meet Specialist Physiotherapy Practitioner, Nicky…
Nicky Williams has an extra special role at Blackpool Victoria’s Critical Care department.
As of of only a few Specialist Physiotherapy Practitioners in the area, Nicky looks after the long-term patients in the Intensive Care Unit, a role she has been performing for the last six years.
Intensive care is needed if someone needs close monitoring after elective surgery or if they become critically unwell and need intensive medical.
A person can lose up to 8% muscle mass in just one day, so the earlier we can start the rehab, the better for the patient.”
Once patients’ conditions have improved within Intensive Care, they are often transferred to the High Dependency Unit (HDU). The HDU ward is for patients who need more intensive observation, treatment and nursing care than is possible in a general ward, but slightly less than that given in Intensive Care.
“But I feel very lucky and privileged. I get to know patients and families so well throughout the process. It is very sad that not all the patients recover and that does take its toll at times, but it’s so rewarding to see people recover and go on to live their lives.”
Meet our Critical Care Lead for The Emergency Village and Critical Care Development
Dr Rob Thompson is a Critical Care Consultant at Blackpool Victoria Hospital and is also the Critical Care Lead in the Emergency Village and Critical Care Development.
He qualified as a doctor in 1999.
Rob is the first doctor in his family. Originally from Shropshire he studied medicine at the University of Manchester.
Rob came to Blackpool Victoria as a junior doctor and thought it was a nice place for staff and so he stayed. This is also where he met his wife, a nurse.
Through specialist training programmes, he went on to train in anaesthetics and Intensive Care, starting his current role in 2010.
He said: “I have always wanted an interesting and rewarding career and for me, that is medicine.
“I enjoy being hands on and in Critical Care; you can see immediate effects which is very satisfying.
“The job can be emotionally draining and it never gets easier although we do have a lot of coping techniques. However, it is amazing to see patients in follow up clinics once they are better – some have completely transformed.”
Rob is one of the Critical Care consultants who have overall responsibility for the care delivered across the Intensive Care Unit (ITU) and the High Dependency Unit (HDU) which make up the 16 beds of ‘critical care’.
The Emergency Village and Critical Care development will see ITU and HDU come together in a new purpose-built building alongside the current Urgent Care Centre. Currently, these wards are in separate areas of the hospital.
Rob said: “Critical care is very traumatic and the environment can aggravate families who are already distressed.
“The new location will provide more privacy and dignity by providing separate rooms which will help lessen the distress.
“There will also be more room to rehabilitate our patients to get them get back home and managing their daily routine.
“Through a focus group of former patients and their families, we asked about their experiences and suggestions. We listened to this and will now provide an enhanced relatives’ room and facilities with provision for overnight stays.
“Combining ITU and HDU will provide a much more enhanced environment for the patient to get better especially regaining the ability to look after themselves.
“The whole team are excited about the changes and are looking forward to working within a space that they all have put ideas into in order to make the patient care the best that it can be.”
Back to the floor for consultant Jason
A Critical Care Consultant has spent a shift as a nurse in order to get a better understanding of their role.
Dr Jason Cupitt, who works at Blackpool Victoria Hospital, spent the day on the Intensive Care Unit performing the duties of a staff nurse.
He said: “I watched an interes
ting online talk by Neil Spenceley, National Patient Safety Lead for Paediatrics, in which he spent time in a variety of roles and which gave him a new understanding of specific issues and challenges in the work place in order to better understand the whole picture.
“Sometimes the way teams interact can be toxic. I’ve found that incivility is widespread in healthcare. And poor behaviours affect patient safety. I wanted to see first-hand what pressures the nurses face and the many parts of their job that the consultants don’t see.”
Jason’s shift was supported by Staff Nurse Malissa Paterson on an exceptionally challenging day with a sick, deteriorating patient.
He said: “I didn’t realise how much paperwork was involved on a daily basis. It seemed relentless. I was very humbled by how much the nurses have the doctor’s back. And how they are the eyes, the ears, the advocate of the patient. Not only are they dealing with the patients but also their families which can often be emotionally challenging. I realised that the doctors tend to parachute in, bark out orders, and leave in a cloud of smoke. The nurse is by the bedside for a solid 12 hours.
“After my experience, I am now looking at what we can do as a consultant body to better support the whole team, build their confidence and improve output. We can target recruitment and retention and good people won’t leave.”
Unit Manager for Critical Care, Lauren Snape, said: “If only every workplace had a Dr Cupitt.
“Jason is exceptionally supportive of the nursing workforce not just in our team but in the Trust. Following some members of the team watching Neil Spenceley’s video, I challenged Dr Cupitt to become a nurse for the day. In true style it took him less than a minute to accept the challenge!
“The nursing team were exceptionally responsive and welcoming to this new experience. I think it is fair to say in the lead up to his shift it lifted spirits and was a new and exciting concept. We had no real plan of how it would work or what his level of participation would be. I must say he did exceptionally well at staying focused and reminding our medical colleagues he was there as a nurse and that’s how he wanted to be seen that day.
“Dr Cupitt has demonstrated he will go above and beyond for the nursing staff. We see how committed he is and we know he genuinely wants us to have a positive workplace culture. I want to reinforce he is doing an exceptional job of this.”
May 2018
Blackpool Victoria Hospital welcomes an off the hoof visitor
Blackpool Victoria Hospital welcomed a special visitor who put the ‘whinny’ into Whinney Heys Road.
One year-old American miniature horse, Digby, is the first guide horse in the UK and is one of a small number of therapy horses across the country. He dropped in for a special visit to be ‘neigh’bourly to staff and patients.
Two foot tall Digby was accompanied by Katy Smith, owner of KL Pony Therapy in Northallerton, who has 30 years of experience working with horses.
She said: “Our ponies are trained to be social and they create lovely memories for the patients they meet, particularly if they are feeling fed up.
“The miniature horses can live up to 50 years, which makes them ideal as guide horses for the blind and partially sighted. They enjoy doing visits and love to meet people.”
Digby’s visit was arranged by doctor and horse rider, Emma Jackson. She said: “I had heard of the ponies visiting hospitals and care homes and thought it would be a great idea for the horses to visit our Critical Care Unit among others.”
Digby proved a real hit with patients as does the therapy dog, Dandy, who visits the Critical Care Unit every week.
Critical Care Consultant, Dr Jason Cupitt, paid for Digby’s visit himself because of the healing qualities that animals can bring to patients.
He said: “We know that animals have been proven to aid psychological wellbeing as we have seen with the regular therapy dog visits.
“Sometimes a visit from an animal is just what a patient needs to get well again. And who can’t relate to a lovely animal like a dog or a horse?”
Digby’s colleague, Mr P, a yearling, also visited the Unit then went on to visit the Children’s Ward for a little horseplay.